Your Doctor Doesn’t Want You to Have a Birth Plan?
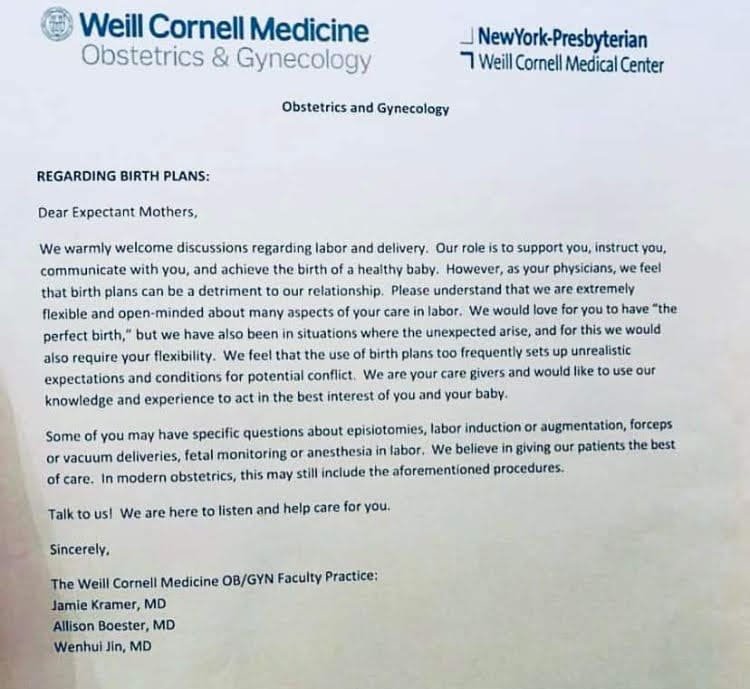
In June 2022, a letter an obstetric practice in New York sends to their patients was published online.
The text of the letter reads:
“Dear Expectant Mothers,
We warmly welcome discussions regarding labor and delivery. Our role is to support you, instruct you, communicate with you, and achieve the birth of a healthy baby. However, as your physicians, we feel that birth plans can be a detriment to our relationship. Please understand that we are extremely flexible and open-minded about many aspects of your care in labor. we would love for you to have "the perfect birth," but we have also been in situations where the unexpected arise [sic], and for this we would also require your flexibility. We feel that the use of birth plans too frequently sets up unrealistic expectations and conditions for potential conflict. We are your care givers and would like to use our knowledge and experience to act in the best interest of you and your baby.
Some of you may have specific questions about episiotomies, labor induction or augmentation, forceps or vacuum deliveries, fetal monitoring, or anesthesia in labor. We believe in giving our patients the best of care. In modern obstetrics, this may still include the aforementioned procedures.
Talk to us! We are here to listen and help care for you.
Sincerely,
The Weill Cornell Medicine OB/GYN Faculty Practice:
Jamie Kramer, MD
Allison Boester, MD
Wenhui Jin, MD”
Unfortunately the OBs who signed this letter are not unique in their dismissal of birth plans as “detrimental.”
Just to be clear: There are many OBs and nurses who are extremely respectful of birthing people’s preferences. We are not making blanket statements here, but talking about the subset of these professionals who are antagonistic toward birth plans and the people who create them.
A few other words we’ve heard from OBs, nurses, and even hospital-based midwives to describe birth plans are “unreasonable,” “disrespectful,” and “naïve.”
It’s no coincidence that these sentiments are so prevalent in a country with some of the worst perinatal mortality rates in the developed world - not to mention a high cesarean rate and drastic racial inequities in birth outcomes.
Why is this? Why do hospital-based medical professionals so often feel this way?
It’s clear that there is a disconnect between the way birthing people perceive the purpose of birth plans, and the way hospital clinicians often do.
What clients think birth plans do:
Provide an opportunity to learn more about what their options are and what choices they would prefer to make in various scenarios that may arise during birth
Spark questions to research and/or talk with their care providers about
Provide a tool to help discuss their preferences with their providers ahead of time
Help facilitate communication during labor and birth (usually with unfamiliar people they've never met before) to let their care providers know a little bit about them and what kind of experience they are hoping for
Offer a starting point for conversation if/when surprises happen along the way and choices need to be made
This is why we provide free access to an educational birth plan tool - it’s one of the most popular aspects of our doula package!
What some clinicians think birth plans do:
Encourage parents to "become Dr. Google"
Cause parents to question or dismiss their medical expertise and experience
Convince parents that their birth will be "perfect" if they plan it just right
Lead parents to make unsafe choices in a medical emergency
Disrupt the caregiver/patient relationship
You can see how these differing viewpoints feel very at odds with one another.
On one hand, people giving birth often view birth plans as tools to facilitate learning and communication. And on the other hand, medical professionals often view birth plans as disrespectful and even dangerous.
Clinicians in this camp tend to view a birth plan as just a piece of paper, rather than the learning, intention, and vulnerability that went into creating and sharing it.
So what does it mean if a care provider feels that someone communicating their preferences and asking questions is actually “detrimental” to the caregiver/patient relationship?
We found the perfect summary thanks to stimmyabby:
Sometimes people use “respect” to mean “treating someone like a person” and sometimes they use “respect” to mean “treating someone like an authority.”
And sometimes people who are used to being treated like an authority say “if you won't respect me I won't respect you” and they mean “if you won't treat me like an authority I won't treat you like a person.”
And they think they're being fair but they aren't, and it's not okay.
That really hits home, doesn’t it? It’s all about power dynamics.
Let’s stop and assume that a care provider who prefers their patients don’t create birth plans truly has their patients’ best interests in mind.
Why might a well-intentioned care provider dislike birth plans?
They want patients to be aware that things might not always go as expected
They don’t want their patients to be disappointed if something changes and patients “don’t get everything they wanted” from their birth plan
They see relying on a birth plan as a potential source of birth trauma
From our perspective, this would be the best case scenario if a provider expressed a dislike for birth plans. If a provider has these concerns, they could simply have a conversation with their patient.
Discussing what would happen if things changed and “plan A” wasn’t possible anymore would be a great idea, right? That would give a patient the chance to:
ask more questions about what kinds of situations the provider has in mind so they can learn more, and
let the provider know that they are aware things may change, and that they view their birth plan as a communication tool to help their providers (prenatally and during labor and/or a c-section) understand their overall preferences.
In our experience, having a birth plan is often a way for parents to say, “If something changes, I want to be intimately involved in the decision-making process for what happens next, in collaboration with my care team.”
(Remember: only the pregnant person has the right to make decisions about their body and medical care. Not their partner, doctor, nurse, midwife, doula, etc.)
But the way providers sometimes interpret patients who have a birth plan leans more toward labeling them “non-compliant” or “difficult.”
Making the choice to essentially ban birth plans as the Weill Cornell practice did clearly shows that some providers are not interested in more or better communication with their patients.
It shows that they don’t trust their patients to make the “right” decisions (in their eyes).
It shows that they would rather not explain their reasoning for some of their recommendations.
It shows that they prefer not to be asked questions.
It shows that they do not acknowledge that communication failures lead to worse outcomes for parents and babies - both health outcomes and emotional outcomes.
It shows that they do not understand that the way someone is communicated with prenatally and during labor can lead to trauma.
It shows that they do not understand that their patients retain all of their human rights (PDF download) and decision-making power while pregnant and in labor.
Perhaps most of all, it shows that they do not understand their ethical and legal obligation to give their patients “informed consent.”
According to the American College of Obstetricians and Gynecologists (ACOG):
“Meeting the ethical obligations of informed consent requires that an obstetrician–gynecologist gives the patient adequate, accurate, and understandable information and requires that the patient has the ability to understand and reason through this information and is free to ask questions and to make an intentional and voluntary choice, which may include refusal of care or treatment.
Shared decision making is a patient-centered, individualized approach to the informed consent process that involves discussion of the benefits and risks of available treatment options in the context of a patient's values and priorities.”
- Informed Consent & Shared Decision-Making in Obstetrics & Gynecology, 2021
(emphasis ours)
As birth workers, we are well aware that informed consent conversations almost never look like this - especially with medical care providers who are so dismissive of patients’ wishes and questions that they don’t even want them to have a birth plan.
Let’s revisit this quote from the Weill Cornell letter:
“Birth plans can be a detriment to our relationship.”
As we’ve discussed, many birthing people consider birth plans to be a tool to help them learn about their options and have open conversations with their care providers.
Let’s try replacing “birth plans” in this sentence with “being aware of your options and opening a collaborative conversation.”
Here’s the new sentence:
“Being aware of your options and opening a collaborative conversation can be a detriment to our relationship.”
YIKES. That’s the heart of the matter here.
When a provider views a tool for education and shared decision-making as a threat, they view their patients’ LEGAL RIGHT to ask questions and make choices about their bodies as a threat.
That’s a definite red flag.
The International Cesarean Awareness Network (ICAN) tweeted a great response when this letter went public:
“There, Weill Cornell Medicine, we fixed it for you.
Thanks to Ashe Birthing Services and The Taproot Doula Project for bringing this letter to our attention.
This is not informed consent. This is obstetric violence.”
ICAN’s revised Weill Cornell letter reads:
“Dear Expectant Parents,
We warmly welcome discussions regarding labor and delivery. Our role is to support you, instruct you, communicate with you, honor your human rights, and achieve the birth of a healthy baby and healthy parents. Please understand that we are extremely flexible and open-minded about your care in labor. We would love for you to have "the perfect birth," but we have also been in situations where the unexpected arise [sic], and for this we would do everything we can to support your physical, spiritual, and emotional health. We feel that the use of birth plans gives us the opportunity to learn about you as a person and what matters to you. We are your care givers and would like to use our knowledge and experience to act in the best interest of you and your baby.
Some of you may have specific questions about episiotomies, labor induction or augmentation, forceps or vacuum deliveries, fetal monitoring, or anesthesia in labor. We believe in giving our patients the best of care. Our own ethical guidelines in obstetrics allow us to include the aforementioned procedures if we follow a rigorous process called "informed consent" that means the decision is ultimately always yours.
Talk to us! We are here to listen and help care for you.
Sincerely,
The Weill Cornell Medicine OB/GYN Faculty Practice:
Jamie Kramer, MD
Allison Boester, MD
Wenhui Jin, MD”
If your care provider’s approach is more like the original letter than this revised version, we strongly encourage you to consider finding a more supportive, patient-centered clinician to work with.
If you need suggestions, reach out to doulas in your area - we usually have a go-to list of respectful caregivers in the area where we practice.
Get our free guide:
Pack the Perfect Hospital Bag